Are your teeth at risk of tooth decay or tooth wear? In this post we explain how tooth surfaces are affected by what we eat and drink and what you can do to help keep your smile in tip top shape.
Are you at risk?
Do you –
- suffer from dry mouth (or take medication that causes dry mouth)?
- graze rather than eat at specific mealtimes?
- eat/drink before bedtime?
- take medication that is sugar based or causes dry mouth?
- have gum recession?
- have a lot of old/large fillings?
- struggle to clean your teeth thoroughly?
- use high calorie nutritional (dietary) supplements?
- use methadone?
Have you –
- had tooth decay in past two years?
- poorly mineralised teeth/tooth surfaces?
- partly erupted wisdom teeth that are hard to clean?
- partial dentures or an orthodontic appliance?
Yes? You may be at higher risk of tooth decay or tooth wear.
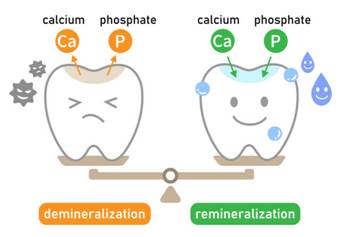
If you follow Growing Smiles on social media you may have noticed the post about Stephan curves. Stephan Curves show what happens to the pH in our mouths when we eat/drink. The pH in our mouth is important as it can lead to loss of tooth surfaces by a process called demineralisation (dissolving tooth surfaces). Our mouths are in a constant see-saw motion between demineralisation and remineralisation (re-hardening of the surface).
Enamel is the outer covering of our teeth and the hardest substance in the body. Dentine is the layer beneath the enamel and makes up the majority of the tooth surrounding the pulp chamber which houses the nerves and blood vessels.
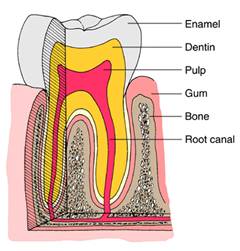
When pH drops to 5.5 or below enamel will start to dissolve (demineralise), dentine starts to demineralise around pH6.4. This means exposed dentine e.g. on root surfaces are at increased risk from acid attack. The longer teeth remain in ‘danger zones’ of acid attack where demineralisation occurs, the more damage to teeth.
While there are other causes of tooth surface loss (tooth wear), tooth surfaces demineralise most commonly as a result of tooth decay (dental caries) or acid erosion.
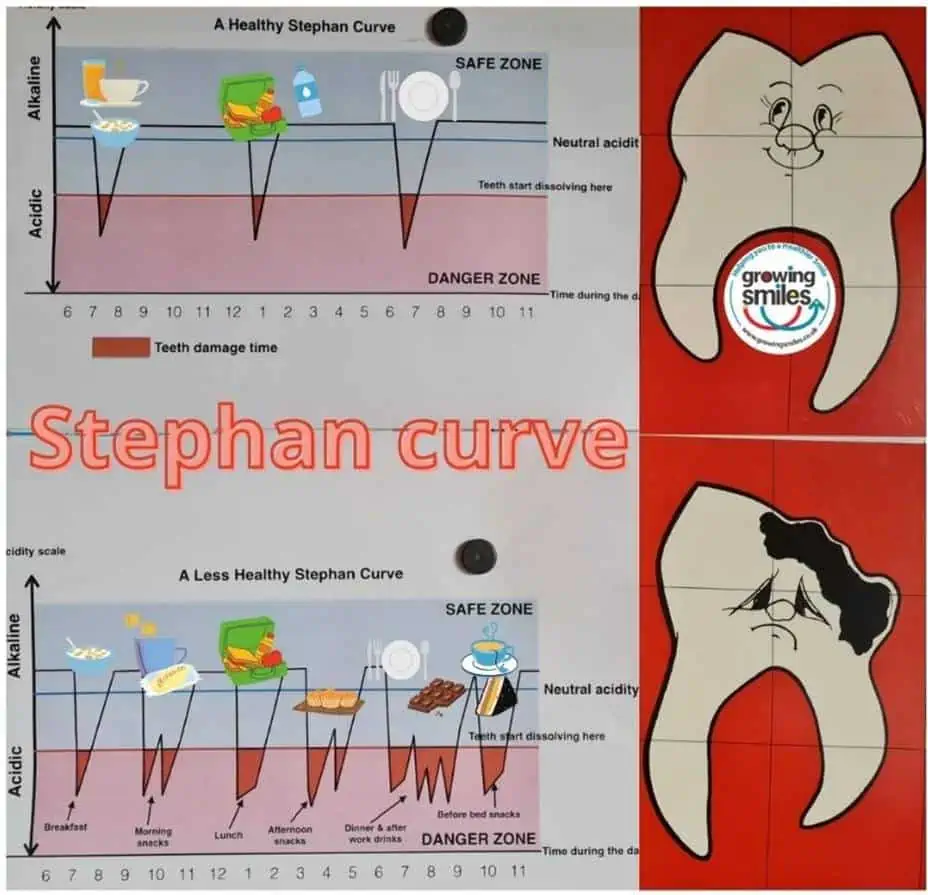
Bacteria in dental plaque digest dietary sugars (particularly free sugars) to produce acids = pH drop. These acids demineralise the tooth surface and over time the result is a cavity (tooth decay). As the pH rises calcium phosphate ions remineralise the tooth surface. The more time teeth spend in ‘danger zones’ without enough time between acid attacks for tooth surfaces to remineralise, the more damage will occur.
The difference between tooth surface loss from acid erosion and tooth decay is the presence of bacteria in the plaque biofilm. Erosion occurs without bacterial plaque present. Acids from the stomach or from the diet – e.g. food/drink, but also medication and supplements (anything with low pH), come in contact with tooth surfaces = demineralisation. Erosion is also affected by titratable acidity. Titratable acidity is the effort required to return pH to a neutral/safe environment. The higher the titratable acidity the longer it takes for pH to return to neutral.
So what restores pH in the mouth?
A process called remineralisation is the natural repair process for teeth. Think of it as hardening the tooth surface after acid attack.
Saliva is extremely important in the process of recovering a neutral pH to the mouth by remineralising (hardening) tooth surfaces after acid attack. Calcium and phosphate minerals are depositing back into the tooth surface by saliva. Lack of saliva or saliva that is thick, ropey or sticky increases the risk of developing tooth decay (caries) and/or erosion.
Tooth surface either from decay or erosion is a balancing act between how long the teeth are bathed in acid v the time it takes for the teeth to recover and stay in the ‘safe’ zone.
Key influencers for tooth decay
Diet – too much decay causing sugar, too often
Lack of fluoride around teeth
Lack of saliva and its buffering capacity

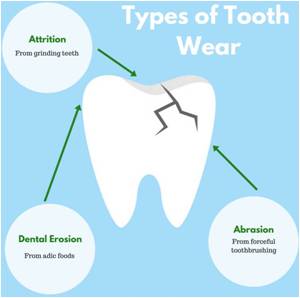
Non decay related tooth wear is related to various factors. It is important to identify the cause of tooth wear to ensure appropriate management.
Maintain a healthy environment in your mouth.
- Eat a healthy diet at regular mealtimes. Avoid ‘grazing’ throughout the day.
- Eat a ‘remineralising’ calcium and fibre rich diet e.g. plain milk, yoghurt, low fat cheese. Fruit and vegetables encourage saliva flow.
- Keep sugary and acidic food and drink to mealtimes and avoid them before bedtime when your saliva production is reduced.
- Avoid acidic drinks e.g. soft drinks, fruit juices
- Drink plain water which helps prevent dehydration and dry mouth.
- Don’t brush teeth immediately after acidic food/drink or after vomiting when tooth surfaces are softened by acids and more prone to wear. Leave 45-60 minutes. Instead use an alcohol free fluoride mouth rinse, chew sugar free gum, rinse with water or apply a reminerlising paste.
- Use low abrasive toothpaste containing 1,350 to 1,500ppm fluoride or a toothpaste designed to protect against acid attack, at least twice a day. Before bedtime and in the morning. Spit out after brushing but don’t rinse with water to avoid diluting the fluoride concentration.
- Regularly ‘moisturise’ tooth surfaces with a remineralising cream.
- Cleaning between teeth daily before brushing or at a different time of day. Often cavities develop on the surfaces between teeth where your toothbrush can’t reach.
- Chew sugar free gum with xylitol after eating and drinking.
- Use an alcohol-free fluoride mouth rinse at a different time to brushing.
- If you suffer from a medical condition that causes acid reflux e.g. gastric reflux, eating disorder etc speak to your Doctor.
- Check any medications taken regularly are acid (e.g vitamin C, aspirin, iron preparations) and sugar (e.g. liquid lactolose or morphine)free. Take these at mealtimes if possible.
- Use products that aid remineralisation to harden and protect tooth surfaces e.g. contain fluoride, casein phosphopeptide, xylitol.
Speak to your dentist to find out if high fluoride toothpaste, topical fluoride therapy or fissure sealants are appropriate.

Not sure of your risk?
Take ‘My Dental Score’ free to identify your personal risk of tooth surface loss.
Would you like some help from an expert?
Use LiveChat to contact us for advice and options for one to one coaching.


