Saliva plays a very important role in oral health and is often not appreciated until it’s not there (dry mouth). Saliva buffers and helps to neutralise acids and sugars in your mouth and coats the soft tissues protecting them from trauma when eating, swallowing, and speaking.
So why is saliva so important?
- it is the first line of protection against bacterial invasion
- helps to wash away food and debris from teeth and gums
- moistens and breaks down food for chewing, swallowing and taste
- provides disease-fighting substances to help prevent cavities and other infections
- helps to neutralise acids produced by bacteria in the mouth and keeps tooth surfaces strong by providing calcium, fluoride and phosphate ions. These help remineralise (heal/harden) tooth surfaces after sugar and acid attack
- helps maintain the pH of the mouth
Simply – it is your secret helper!
Chronic dry mouth increases your risk of developing tooth decay, gum disease and bad breath (halitosis). It is very unpleasant and can seriously impact your overall quality of life. It can affect speaking and taste, chewing and swallowing, which in turn affects nutrition and potentially your general and oral health.
If you suffer from dry mouth you may also experience symptoms such as; a burning sensation or soreness in your mouth, dry lips, reduced or altered sense of taste, recurrent mouth infections e.g. oral thrush, poor fitting or uncomfortable dentures or oral appliances and/or trauma and ulcers from tissues rubbing on teeth, dentures etc.
What is going on?
Dry mouth is a symptom, not a disease. If your mouth is dry it is important to identify the cause, so that it can be treated and managed properly. Your dentist or doctor can help with this.
Everyone’s mouth gets dry mouth on occasion e.g. if you are dehydrated or nervous. Many people notice their mouth dry in the morning when they wake up. This can be related to ‘morning bad breath’, which is quite normal and disappears rapidly when saliva is produced as you ‘get going’- eating, drinking and speaking. It can be more noticeable if you breathe through your mouth rather than your nose, especially at night. Drinking alcohol will dehydrate and increase oral dryness. If you use CPAP or oxygen therapy this will also cause dry mouth.
Basically it means your salivary glands aren’t producing enough saliva. Often this is because you are dehydrated and your body just doesn’t have enough fluid to produce the saliva you need.
Tip – drink plenty of water/fluids to prevent dehydration, however, bear in mind that if your mouth is continually dry it can be an indication of an underlying health problem.
See more about saliva and its role on oral health here.
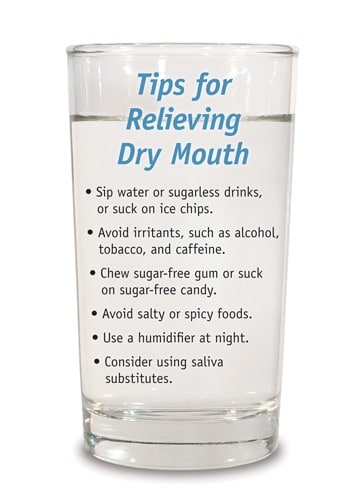
Tips for Relieving Dry Mouth
Several factors can impact the production of saliva. These include:
Medications – lots of medicines can cause a dry mouth, e.g. antidepressants, antihistamines and diuretics. Some of these may have been prescribed by your doctor, or you may have bought them over the counter from a pharmacist or supermarket. Check the leaflet that came with the medicine to see if dry mouth is listed as a side effect.
Mouth breathing – breathing through your mouth rather than your nose either at night or during the day can cause your mouth to dry. This can be short term e.g. if you have a cold and have a blocked nose or long-term mouth breathing.
Diabetes – It is a common symptom of both type 1 and type 2 diabetes. The exact reasons are unknown, but high blood sugar levels could cause dry mouth in people with diabetes. Some medications used to treat diabetes can have a side effect of dry mouth. See our specialist oral health care range for diabetics here.
Radiotherapy or Chemotherapy – Treatment to the head and neck can affect the salivary glands, reducing the amount and quality (very thick and difficult to swallow) of saliva, even to the extent of having no saliva. After treatment it can take a long time (6 months or more) for saliva production to return to normal, but if treatment has directly affected the salivary glands you may permanently have dry mouth and related problems.
Sjögren’s syndrome – a condition where the immune system attacks and damages the salivary glands and other moisture-producing glands e.g. tear secreting glands.
CPAP or Oxygen therapy can increase oral dryness. We recommend Xylimelts to reduce symptoms and side effects of dry mouth. Find out more here.
Anxiety – this can have short or long term effects.
High salt or sugar in your diet.
There are a number of conditions where a dry mouth may be a problem. Patient information for a number or oral conditions can be found on The British & Irish Society for Oral Medicine (BISOM) website.
What you can do –
Daily, effective oral hygiene is key to maintaining oral health and fresh breath – e.g interdental cleaning, tooth brushing etc. Find out more here.
Talk to your doctor or dentist about the cause and what is best for you to relieve symptoms.
Take regular sips of water throughout the day.
Chew sugar free gum or suck sugar free sweets to stimulate saliva flow.
Use products specifically for relief of dry mouth e.g. artificial saliva substitutes, mouth gels, toothpastes etc. See our range of products for dry mouth here.
Xylimelts – popular for dry mouth
Use products that help protect tooth surfaces such as Tooth Mousse or MI Paste Plus.
Avoid alcohol (including alcohol-based mouthwashes), caffeine and smoking – these can all make a dry mouth worse. See our alcohol free mouthwashes here.
Visit your dental team regularly, who may:
- Recommend a high fluoride toothpaste and/or fluoride mouth rinse
- Apply topical fluoride
- Advise you to see the dental hygienist/therapist for preventive therapy regularly
Recommend saliva stimulants – sugar free and non-acidic .